Reflecting on Dr. Suen’s Teaching Experience
14
Dec
2023
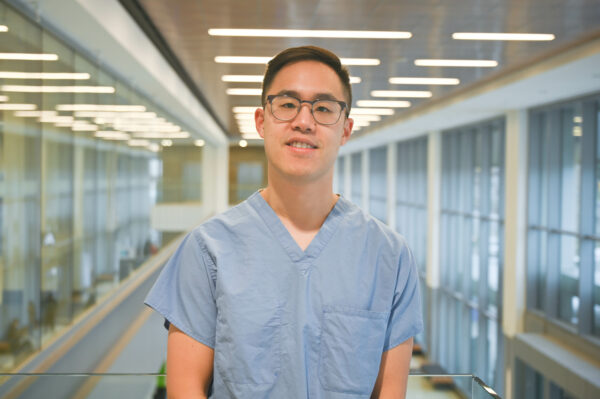
In the past year, Humber River Health (Humber) had the privilege of hosting over 40 residents from prestigious institutions like the University of Toronto, McMaster University, and Queen’s University. Dr. Colin Suen, an Anaesthesiologist at Humber, teaches in the Department of Anesthesia and Pain Medicine at the University of Toronto and was recently recognized by the university for his overwhelmingly positive teaching evaluations.
Through achieving a perfect score in his evaluations, standing well above the average in comparison to other sites, Dr. Suen provides effective clinical teaching that stimulates learners to build knowledge and skills safely. Dr. Suen reflects on his teaching experience below.
What are qualities that define an excellent teacher in your field?
In Anesthesia, our interaction with learners takes place primarily in the operating room. We often spend the whole day supervising a learner, so the level of interaction and engagement with residents or students is quite high. We supervise a wide range of learners including residents in Anesthesiology, Emergency Medicine, Critical Care, Oral Surgery, as well as Medical students, Respiratory Therapist students, and Anesthesia Assistant students. Some of the qualities I believe are important are patience, approachability, adaptability to different learning styles, good communication, and being receptive to feedback.
How do you engage your students in active learning?
I think it is important to set goals and expectations at the beginning of the day. If I have not previously worked with the learner, I will ask about their stage of training, recent clinical rotations, and gauge their comfort level with the type of cases and any relevant technical skills. I will ask the learner to identify their learning objectives for the day, which may be clearly defined like practicing a specific procedure, or more generalized and observational. I will also ask about any formal assessments such as Entrustable Professional Activities (EPAs) for trainees in Competency Based Medical Education (CBME) programs and other workplace-based assessments to ensure I can appropriately observe for milestones and be available to complete them.
Before each case, I will review the resident’s anesthetic plan to identify case-specific considerations and goals. This is an opportunity to discuss any missing steps or knowledge gaps, and to use them as teaching opportunities later in the day. In addition, it helps with cognitive priming for when problems or complications arise. Otherwise, my goal is to allow the learner to execute their plan as autonomously as possible and to provide minimal intervention. There are many ways to conduct anesthesia, so I aim to be flexible and open-minded to new methods, as long as they are safe and the learner understands the pros and cons. I often end up learning new things, another rewarding aspect of working with learners.
At the end of the case, or end the day, I will debrief with the learner to review what went well and what could have been improved. Feedback is best when it is timely. I let the learner guide the self-reflection before offering my observations and suggestions for improvement. The feedback goes both ways, as this is also an opportunity for feedback as a teacher.
What steps do you take to create a supportive and inclusive learning environment?
The operating room (OR) can be an intimidating place for learners. The environment, equipment and people can all be unfamiliar. At the beginning of the day, I will orient the learner to the OR and the facility and introduce them by name, type of trainee, and their stage of training to the perioperative team so that their role is clear. It is also important to ensure psychological safety by being approachable, available, and encouraging learners to ask questions without fear of judgement. I try to focus on giving constructive feedback, making sure to celebrate and acknowledge successes to reinforce positive behaviour, and boost confidence. When errors occur, it is part of the learning process. I avoid being overly critical, especially in front of other perioperative team members. Instead, I try to normalize the experience, for example, by sharing a personal experience of my own mistakes.
Finally, I try my best to make sure learners feel appreciated. Residents are working hard and long hours in the hospital, spending their free time studying. Small gestures like buying coffee or lunch can go a long way.
How do you incorporate technologies or innovations in your teaching?
There are some great online resources for certain skills, such as peripheral nerve blocks for anesthesia. I use YouTube and mobile apps that are excellent for illustrating the anatomy and ultrasound images for regional techniques. This is especially useful when a learner is acquiring a new technique they are not familiar with. There are also apps and interactive simulators developed at the university for point of care, ultrasound and bronchoscopy.
