Command Centre Clinical Tile Series: Newborn Assessment Tool
01
Sep
2020
The first few hours after the birth of a child is crucial. This period is a transitional phase, in which the newborn is adapting to life outside of their mother’s womb. Therefore, it is critical to identify, interpret, assess and reassess potential risks as soon as possible. Humber River Health has developed a Newborn Assessment Tool that assesses a newborn’s risk of deterioration and lessens the separation with their mother. The tool went live on July 28.

The Newborn Assessment Tool is a digital system that can be accessed by staff on the front lines at any time. Factors such as temperature, heart rate, respiratory effort and oxygen saturation are the types of objective measures that are inputted into the system. When evaluating their patients, staff record data regarding the mother and their newborns into patient monitors which feeds into the hospital’s Electronic Medical Record (EMR). To determine if the baby is at risk of deteriorating, the tool evaluates this data, along with additional notes made by the nurse or physician to generate a result. Results of the Newborn Assessment Tool are displayed on the Perinatal Tile, which is one of the many tiles that make up Humber River Health’s Command Centre. Staff in the Command Centre, as well as staff all around the hospital, can view the tile.
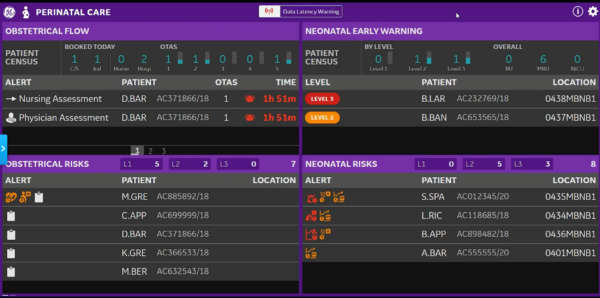
The Newborn Assessment Tool specifically functions within the Neonatal Early Warning section of the Perinatal Tile. The purpose of this section is to give clinicians, team leaders and registered practitioners a broader awareness of what is going on with their patients, as well as allow staff in the Command Centre to centrally monitor these patients and intervene if front-line staff require assistance. By considering patient data, the Newborn Assessment Tool produces an overall score and corresponding level for each newborn patient. A newborn is assigned either Level 1, 2 or 3 which are represented on the tile as either green, amber or red, respectively.
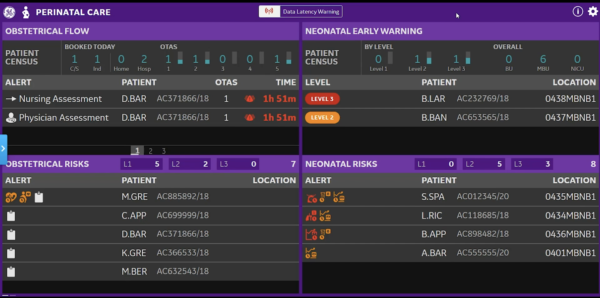
Level 1 indicates that all of the patient’s parameters are within normal range. Staff are aware of Level 1 patients, but they do not appear on the tile as having patients with completely normal parameters would be impractical and overpopulate the tile. The tool only highlights the patients flagged as Level 2 or 3 as they require additional monitoring. When a patient appears on the tile, physicians are called to assess the best course of action with other front-line staff. Once the appropriate response has been made and a staff reassesses parameters, the patient will disappear from the tile. If at any time, a nurse suspects that the newborn is at a greater risk than their level indicates, they may stay by the patient’s bedside and contact team leaders, physicians or other nurses via their Ascom phones for assistance. Even for Level 1 patients, staff have the ability to go into the Newborn Assessment Tool and alter required needs if they feel that their patient is at a higher risk than their level may suggest. On the sample tile above, there is one neonatal patient displaying a Level 2 and another patient with a Level 3. By clicking on the patient on the tile, the user can view details of the patient’s condition, including the parameters that are putting the patient at risk and the factors that determined the patient’s level.
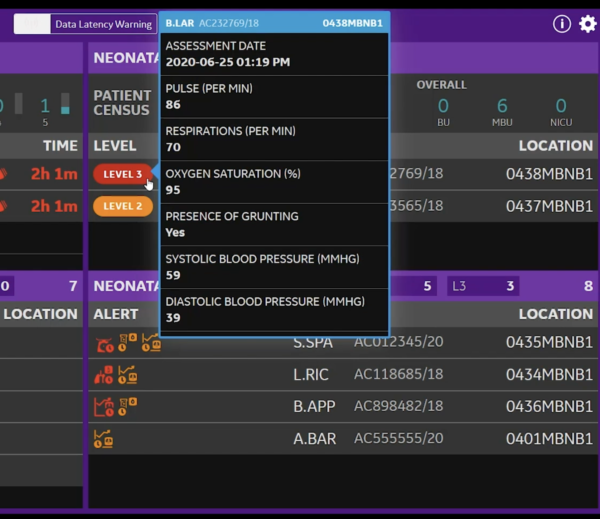
Newborn babies have a lot of work to do transitioning outside of the uterus, as they must maintain physiological parameters such as their temperature and glucose levels. Therefore, a newborn’s vital signs are taken to be the baseline gauge of the newborn’s health status. Typically, a newborn is assessed every 30 – 60 minutes for vitals like temperature, respiratory rate and heart rate. Approximately 4-6 hours after birth, a healthy newborn is reassessed every 6-8 hours.
An example of an abnormal parameter that would trigger the Newborn Assessment Tool is a temperature alert. On average, the oral temperature of a newborn is approximately 36.6°C-37.5°C. If the patient’s temperature exceeds this, this may indicate an infection and a physician must be called to conduct an evaluation. A lower than normal temperature is more common, as babies cannot regulate their body temperature and cannot adjust to temperature changes as well as adults. It is important that newborns are kept at a stable temperature, since they lose heat quickly and are forced to reach into their limited energy reserves to increase their body temperature. If staff view this on the tile, they can brainstorm together and determine the appropriate next steps. In this case, staff might try and use blankets or skin-to-skin contact to increase the newborn’s body temperature. Skin-to-skin contact is a method where the newborn is placed in direct contact with their mother or other caregiver-facing chest-to-chest in an effort to stabilize their temperature. Studies have also suggested that skin-to-skin contact improves sleep patterns, decreases crying and stabilizes blood glucose concentrations.

Another issue that the Newborn Assessment Tool may flag are a patient’s glucose levels. In the sample tile, the data indicates that the newborn has low a glucose level, as it is below a normal blood glucose concentration of 2.5 mmol/L. A solution that nurses could suggest is encouraging the mother to try breastfeeding, or in the case the baby is not latching properly, they could be given a glucose gel mixture orally. Alternatively, glucose could be given to the newborn intravenously.
The Newborn Assessment Tool also uses maternal risk factors, so if the mother has a pre-existing condition, the tool considers the data and produces an alert if it detects that the mother’s condition may affect the newborn. This is important to take into account as, if the mother has diabetes for example; the newborn baby is more likely to have lower blood glucose concentrations or breathing problems. The tool factors in this knowledge prior to discharge and flags newborns for potential risks.
Once a staff assesses the situation and takes action, it is just as important to reassess and re-evaluate the patient to confirm whether the response was effective or not. Multiple steps could be taken to fix the problems that the tool presents, however, the patient will not disappear from the tile until all parameters are within normal ranges. Staff on the front lines and Command Centre are constantly looking at the tile throughout the day, as the goal is to clear all of the patients from the tile.

Overall, the floor of the Maternal and Child units are a complex system as each room has two patients, not just one. Initial patient assessments are mandatory and straightforward, but the Newborn Assessment Tool and the Perinatal Tile are clinical decision tools that can aid in prioritization and planning. Any nurse would tell you that planning is a big part of their job. Once a plan is made from the initial assessment, a vital step here is reassessments and follow-ups. This is where the New Assessment Tool comes in. It aids in how to assess a situation and to see if the subsequent responses were successful in an effort to take care of the hospital’s most precious patients.
The Newborn Assessment Tool was recently featured on CTV News. Watch here.
